ERCP
Endoscopic Retrograde Cholangiopancreatography (ERCP)
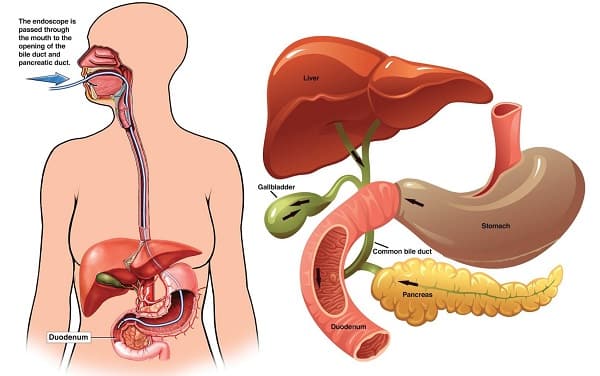
What is ERCP?
Why might I need ERCP?
You may need ERCP to find the cause of unexplained abdominal pain or yellowing of the skin and eyes (jaundice). It may be used to get more information if you have pancreatitis or cancer of the liver, pancreas, or bile ducts.
Other things that may be found with ERCP include:
- Blockages or stones in the bile ducts
- Fluid leakage from the bile or pancreatic ducts
- Blockages or narrowing of the pancreatic ducts
- Tumors
- Infection in the bile ducts
What are the risks of ERCP?
You may want to ask your healthcare provider about the amount of radiation used during the test. Also ask about the risks as they apply to you.
Consider writing down all X-rays you get, including past scans and X-rays for other health reasons. Show this list to your provider. The risks of radiation exposure may be tied to the number of X-rays you have over time.
If you are pregnant or think you could be, tell your healthcare provider. Radiation exposure during pregnancy may lead to birth defects.
Tell your healthcare provider if you are allergic to or sensitive to medicines, contrast dyes, iodine, or latex.
Some possible complications may include:
- Inflammation of the pancreas (pancreatitis) or gallbladder (cholecystitis). Pancreatitis is one of the most common complications and should be discussed with your provider ahead of time. Keep in mind, though, that ERCP is often performed to help relieve the disease in certain types of pancreatitis.
- Infection
- Bleeding
- A tear in the lining of the upper section of the small intestine, esophagus, or stomach
- Collection of bile outside the biliary system (biloma)
You may not be able to have ERCP if:
- You’ve had gastrointestinal (GI) surgery that has blocked the ducts of the biliary tree
- You have pouches in your esophagus (esophageal diverticula) or other abnormal anatomy that makes the test difficult to perform. Sometimes the ERCP is modified to make it work in these situations.
- You have barium within the intestines from a recent barium procedure since it may interfere with an ERCP
There may be other risks depend based on your condition. Be sure to discuss any concerns with your healthcare provider before the procedure.
How do I get ready for ERCP?
Recommendations for ERCP preparation include the following:
- Your healthcare provider will explain the procedure and you can ask questions.
- You may be asked to sign a consent form that gives your permission to do the test. Read the form carefully and ask questions if something is not clear.
- Tell your healthcare provider if you have ever had a reaction to any contrast dye, or if you are allergic to iodine.
- Tell your healthcare provider if you are sensitive to or are allergic to any medicines, latex, tape, or anesthesia.
- Do not to eat or drink liquids for 8 hours before the procedure. You may be given other instructions about a special diet for 1 to 2 days before the procedure.
- If you are pregnant or think you could be, tell your healthcare provider.
- Tell your healthcare provider of all medicines (prescribed and over-the-counter) and herbal supplements that you are taking.
- Tell your healthcare provider if you have a history of bleeding disorders or if you are taking any blood-thinning medicines (anticoagulants), aspirin, ibuprofen, naproxen, or other medicines that affect blood clotting. You may be told to stop these medicines before the procedure.
- If you have heart valve disease, your healthcare provider may give you antibiotics before the procedure.
- You will be awake during the procedure, but a sedative will be given before the procedure. Depending on the anesthesia used, you may be completely asleep and not feel anything. You will need someone to drive you home.
- Follow any other instructions your provider gives you to get ready.
How can we help you?
Contact us at the Gastro World & Liver Centre Rewa (MP) Or make an appointment online.